Beating Tendinitis On Your Own (Part 1)

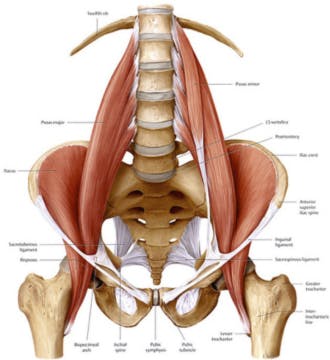
Writing this month’s article has been a difficult task. It started out as an article geared towards helping dancers understand, recognize and assist in treating anterior hip pain. As more dancers entered the Center the last two months with hip, knee and ankle pains I realized they were all fighting the same problem… tendinitis. Therefore, I decided to make an executive decision. We would scrap the article that was previously being worked on and focus on tendinitis, in three phases, to address the cause, prevention and treatment. The fundamental issue of tendinitis is the same whether it is for the hip, knee or ankle. Due to the length of the article and multiple areas of the body we will be covering we will split this up in 3 parts over the next few newsletters.
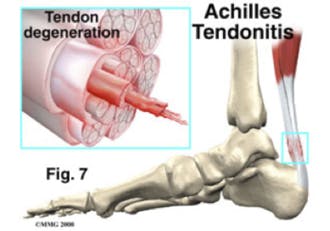
Tendinitis or tendonitis is an inflammation of a tendon, the tough cord of tissue that attaches muscle to bone. It can also be an inflammation of the synovial sheath, a slippery protective layer that surrounds the tendon. Overuse and repetitive rubbing of tendon over bone are the most common causes of tendinitis in dancers. It can also be caused by improper technique, a poor warm up, failure to stretch properly or even following taking some antibiotics.
If you suspect that you have tendinitis the easiest way to self-diagnose it is with a light contraction of the muscle that is affected. You will experience pain and possibly weakness. You may notice pain with palpation of the affected tendon as well. Now because these signs can be positive for several diagnoses it is always advised that you see a medical professional to know for sure.
Ultimately there are 3 great tools that you can use to combat tendonitis. Unfortunately, none of them are things my dancers like to hear.
- The first is rest. Now I don’t know any dancer who views this as a viable option so we always try to come up with alternatives such as avoiding the moves that are causing the most pain.
- The second tool is ice. Frozen peas work great on an affected area for 15-20 minutes at a time every several hours when you are having pain but ice baths work even better. When you completely submerge the joint that the tendon crosses you drop the temperature of all the surrounding tissue and have a better chance at decreasing inflammation.
- Now the third tool is more controversial. Medical Doctors will attempt immobilization of the joint to avoid the rubbing of the tendon and allow it to calm down and in some cases this is very necessary. We, however, have a more active and aggressive approach for some of our dancers. We have the dancer perform eccentric exercises for the tendon in question. This technique is painful and is only utilized when we feel the tendon and the dancer are ready for it. When utilized correctly it is an extraordinary and powerful tool.
Eccentric exercises are the lengthening of a muscle while still contracting it. For instance if you were to perform an eccentric exercise for the hip flexors you may perform développé à la seconde, hold it and then lower it down to the ground very slowly. It causes a “ripping” of the tissue at a microscopic level and leads to a more rapid build up of healthy tissue. This will strengthen the tissue faster than conventional strength training. Unfortunately the process is more painful than normal strength training and therefore our dancers usually grimace at the idea of doing these exercises.
This formula for rehabilitative success can be seen backed up in several studies such as those done by Khan, et al, and Alfredson, et al seen in the references below.
If successful management of the tendinitis is not achieved in 2 weeks with conservative treatment at home, than a deeper look into your condition is warranted by your medical team.
Good Luck and Safe Dancing
References:
Karim M. Khan, MD, et al. Overuse tendonosis, Not tendonitis. THE PHYSICIAN AND SPORTSMEDICINE – VOL 28 – NO.5 – MAY 2000
Alfredson H. Pietilla T, Jonsson P, et al: Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendonosis. Am J Sports Med 1998; 26(3):360-366
